
Life with cystic fibrosis (CF) can often feel like climbing a mountain that never ends. It is a lifetime of uphill challenges, which can vary in intensity. Sometimes the climb is very steep and difficult just to hang on. Other times the incline is less, and maintaining health is more manageable. The newer medications on the market don't necessarily take away the mountain, but they do help us to be better equipped for the challenges ahead!
In these 43 years, I have seen and experienced tremendous advancements in medical treatments including the development of Pulmozyme, Tobi, and now CFTR modulator therapies, including Trikafta, just recently approved by the FDA. With every medical advancement patients of chronic illness (especially rare diseases) are provided better tools for navigating this lifelong uphill challenge, which also contributes to less risk of our health slipping and/or failing, and sticking to the path of prescribed treatments and regimens.
In recent years, insurance companies have been changing their rules and making life with chronic illness once again more challenging.
Two of the insurance imposed policies aimed at cost savings that have negatively impacted me directly are known as "Step Therapy" and "Copay Accumulator Adjustment" programs.
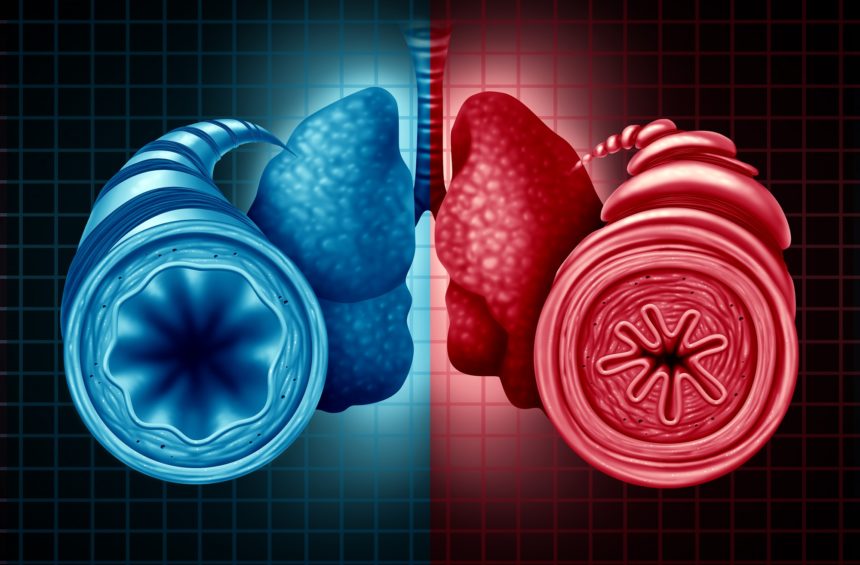
Step Therapy is a process that forces patients onto generic or lower cost medications, even if they have been healthy and stable for a long time on a current medication that might have a higher cost. While sometimes the transition to generic or lower cost option does not create a problem, other times the transition causes significant disruption and a patient must fail on this treatment before being allowed back onto the medication they had originally been stable with. With the mountain climbing metaphor, this would be like taking away your hiking boots and replacing them with slippers until you slip and fall. Then getting your boots back after having all the scrapes and bruises to now also deal with.
This program affected me a few years ago when I was told my insurance would not cover my current insulin until I tried the cheaper alternative. During three months of trying the alternative insulin, I had significantly more trouble controlling my blood sugar, and found my A1C (3-month average blood sugar) had increased to above the dangerous level. I was then allowed back on my original treatment, it took nine months to re-establish my previous A1C level. Was this potential for savings really worth compromising my health for nearly a year?
Copay Accumulator Adjustment programs are another way insurers are trying to drive patients away from brand name (more expensive) treatments and toward generic (lower cost) options. For those of us with CF and other chronic (rare) diseases, we can anticipate to reach 100% of our deductible and out-of-pocket (OOP) maximum, often times within a few weeks or months of a new calendar year. Copays of specialized (Tier-4 or 5) medications which have NO GENERIC OPTIONS are quite substantial, which means a 30-day supply of one single medication can cost between $2,500-$13,000. Many of us rely on help from assistance programs provided by foundations or manufacturers to help us afford such a large chunk of money in order to access our medication. These new programs implemented by insurers say that they will no longer count any "third party" money toward a policy's deductible or OOP maximum. The payment must come STRICTLY FROM THE PATIENT'S OWN POCKET in order to be counted toward the deductible/OOP max. Despite being able to seek patient reimbursement from the assistance programs for these expenses we are being forced to carry, the insurance companies are creating an extremely large barrier to access for many patients and families. With the analogy to mountain climbing, this would equate to being forced to wear a back-pack full of rocks, and having to jump over a very high hurdle to get to your medications on the other side. Because it is a life or death matter, many of us are figuring out how to get that accomplished, with fear that many are not able to, and are forced to go without access to their medications.


As a patient who has and will continue to do everything in my power to live long enough to see a cure to CF in my lifetime, I feel obligated to speak out against these and other policies that make our already difficult lives even more difficult.
Here in Florida, I contacted my state legislators where I am a constituent last May to tell them my story of how these very high copays were only achievable with help, and how I am now being penalized by a policy that says the financial burden of this disease I was born with must lie squarely on my shoulders. Both the Florida House of Representatives and Senate are currently working on various bills that could affect this issue and me in one way or another. I went to Tallahassee this past week to share my real-life story and illustrate to key legislators that these are not just words and numbers on paper. They affect real lives, mine being one of them, and others that are affected much worse than me.
Advocacy is not just about waving a flag and chanting with a group of like-minded people. It is often one voice that is brave enough to share their real story in a way that is meaningful to those making decisions hopefully meant to protect us, the people who elected them. If you are faced with either of these issues, pick up the phone, send an email, or write an actual letter to let your story be known to your representatives and senators. Four states (AZ, IL, VA and WV) have passed legislation banning insurance companies from these types of policies. Could your state be next? Not if no one steps forward about it! Make your voice heard today!


Brian Callanan is now 43-years-old, and was diagnosed with cystic fibrosis at birth. He is the Founder and Executive Director of the CFLF, and practices an active lifestyle primarily through swimming and cycling on and off road, but also enjoys snowboarding, hiking, sailing and rock-climbing. You may email him directly at brian@cflf.org.
***Views expressed in the CFLF Blog are those of the bloggers themselves and not necessarily of the Cystic Fibrosis Lifestyle Foundation***
***Please speak with your physician before making any changes to your CF management***
To continue to receive a weekly blog e-mail and other notifications from the CFLF please click the button below to join our mailing list:
Add new comment